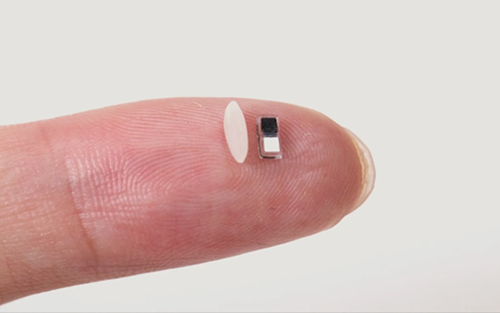
Engineers at Northwestern University have developed the world’s smallest pacemaker, no larger than a grain of rice, that can be injected into the body, provide life-saving cardiac support, and then naturally dissolve. The breakthrough device, described as a “transient” pacemaker, addresses one of the biggest risks in cardiac recovery: complications from temporary pacing wires.
Measuring just 1.8 mm wide and 3.5 mm long, the pacemaker is 23 times smaller than previous biodegradable prototypes. Its miniature size allows it to be implanted via a simple syringe, avoiding invasive chest surgery.
Light-Powered Control: The pacemaker is controlled by infrared light pulses sent from a wearable patch on the patient’s chest, signaling the device when to fire.
Body-Fluid Battery: Powered by a galvanic cell that uses the body’s own fluids, the pacemaker generates electricity without toxic chemicals or external charging.
The “Vanishing Act”: Made from biocompatible materials, the device functions for 5–20 days, the critical recovery window, before safely dissolving into the bloodstream over several weeks.
Traditional temporary pacemakers require wires sewn onto the heart, which must later be removed—a process that can cause internal bleeding. Professor Igor Efimov, co-lead on the study, explained: “The wires can become enveloped in scar tissue. When you pull them out, you risk tearing the heart muscle. Our device eliminates that risk entirely—there is no second surgery because there is nothing left to remove.”
Led by bioelectronics pioneer John A. Rogers, the team sees broader applications for this dissolvable electronics platform:
Pediatric Care: Safe for newborns with fragile hearts.
Nerve & Bone Repair: Electrical stimulation for tissue healing, disappearing after recovery.
Pain Management: Temporary implants could block pain signals before dissolving.
Published in Nature, the study marks a paradigm shift in medical implants—transitioning from permanent hardware to temporary devices that assist the body’s natural healing process and then vanish, reducing risk and recovery time for patients.